A Contemporary Understanding of Low Back Pain
“I've slipped a disc”
“My back is out of alignment”
“I've been told my pelvis is twisted”
These are among some commonly held beliefs that patients carry with them when they first visit Errol Street Physio to get their back pain assessed.
Low back pain presents a monumental disability & financial burden worldwide (1). It affects most of us at some stage in our life, with the vast number of cases being transient in nature.
Unfortunately, a section of the population battles with chronic low back pain over an extended period of time.
Why is this the case?
Over the years low back pain has received some bad press.
Outdated models such as the comments above have entrenched themselves into the human psyche and created fear & “inaccurate beliefs” toward the cause of their pain.
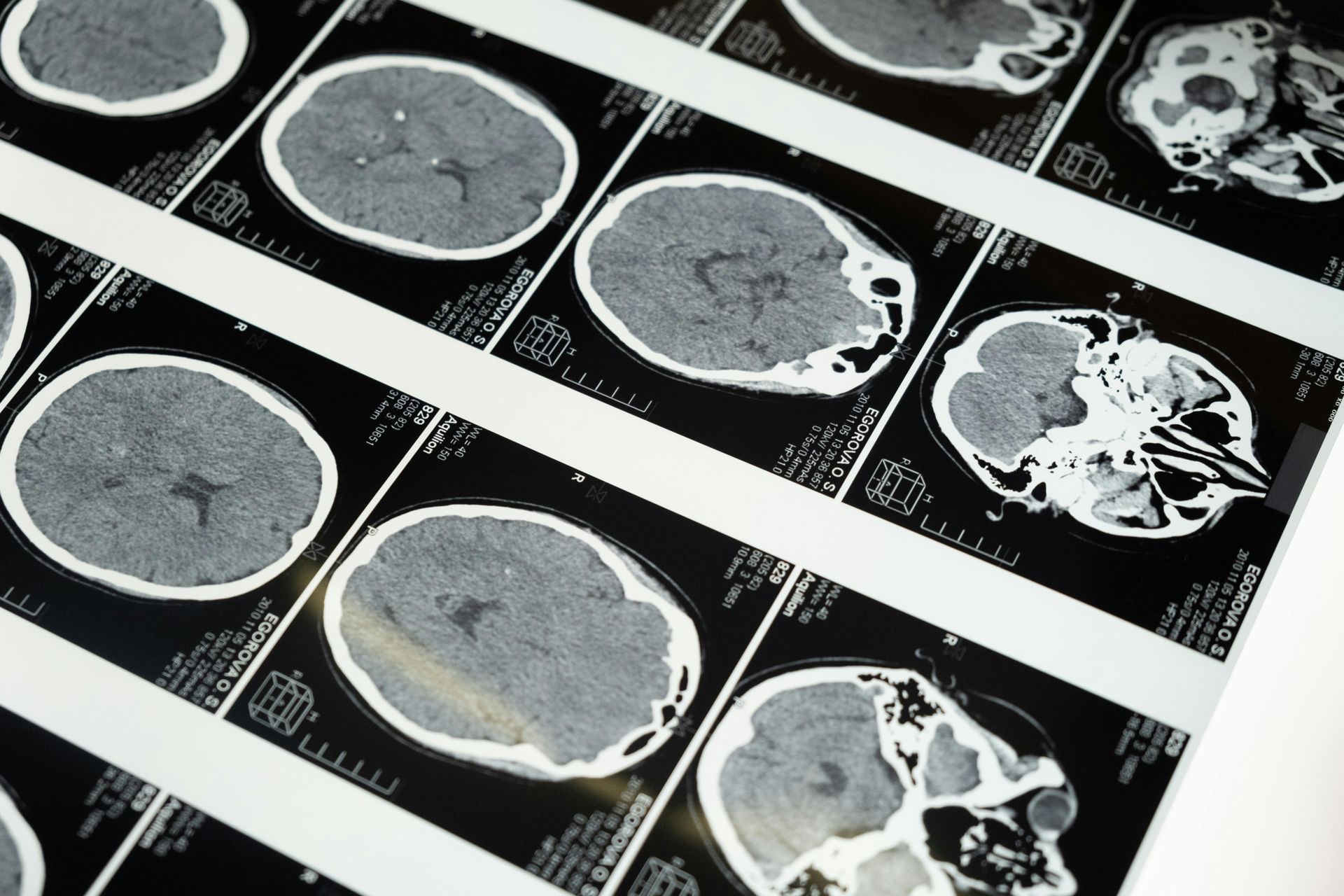
Research has highlighted that abnormal imaging results such as disc bulges, facet joint or disc degeneration are present in people who experience no pain at all (2).
They can sit dormant until pain is experienced, and medical attention is sought.
Individual beliefs and attitudes around their pain experience play a crucial role in the longevity of the back pain cycle.
Say for example, you experience back pain for the first time.
There was no major traumatic episode, but you did some gardening on a Sunday afternoon and the next morning you can hardly move.
The pain persists for a week, struggling to stand up from a chair.
A visit to your medical professional and an MRI later, you learn of 2 disc bulges at L4 & L5.
You are told to rest and avoid bending over at all costs, it will extend the disc bulge.
And……… This is where it is left.
Until 6 months later you still have pain?
Unhelpful narratives contribute to the pain cycle.
Fear avoidance precludes us from moving normally, with the brain placing a “bubble wrap” around the spine, holding it rigid and stiff.
It is this rigidity and stiffness that prolongs the pain experience.
If we consider the narrative around posture:
“Sit up straight, don’t slouch”
“Lift with a straight back”
These all lead to rigidity and a fear of movement.
There has been a growing body of evidence in the contemporary back pain literature that refutes the idea that certain types of static or bending postures can cause low back pain (3).
And……….
Then comes the rise of the core stability empire!
“Your spine is unstable and weak”
“You need to strengthen your core”
Generating a perception that the spine is fragile & weak can lead to further fear avoidance, pain and disability.
So………
Why do we get pain?
Conditioning of the tissues – How accustomed we are to a certain activity – plays a major role in whether we experience a bout of back pain.
The tissue changes that we see on scans, although they are considered normal age -related changes, can at times become a little sensitive and inflamed.
The body reacts with muscle spasm and pain with movement.
The good news here is that if we apply some treatment & education, the tissue sensitivity settles, movement normalises and with some gradual exposure toward the once painful movements, we are back on track!
However…..
Complexity arises in the multi-dimensional nature of chronic low back pain (4)
There are times where the tissue sensitivity might not be the driving force behind your long term back pain.
Feeling threatened, vulnerable & catastrophising about the future, can all feed into a prolonged pain experienced.
As can past experiences such as seeing a relative suffer for years and undergo spinal surgery.
Poor sleep hygiene, fluctuating moods & activity limitations are also in the mix.
This is where the expertise of the Errol Street clinician will really shine through!
For pain that is chronic in nature, we will dig deep to identify if any of these factors are at play.
A comprehensive rehab program for long term back pain will involve, but not limited to:
· Education
· Collaboration
· Empowerment
· Goal setting
· Gradual exercise & activity exposure
Find out more by watching our Youtube video below: