Hips Don't Lie!
Naughties pop star, Shakira, certainly did not suffer with stiff hips! She exhibited a hip range of motion and movement control, that was second to none!
Unfortunately, for the remainder of us less physically gifted, hip stiffness can provide very real issues.
To understand the causes of Hip joint stiffness, it’s important we define what the hip joint is.
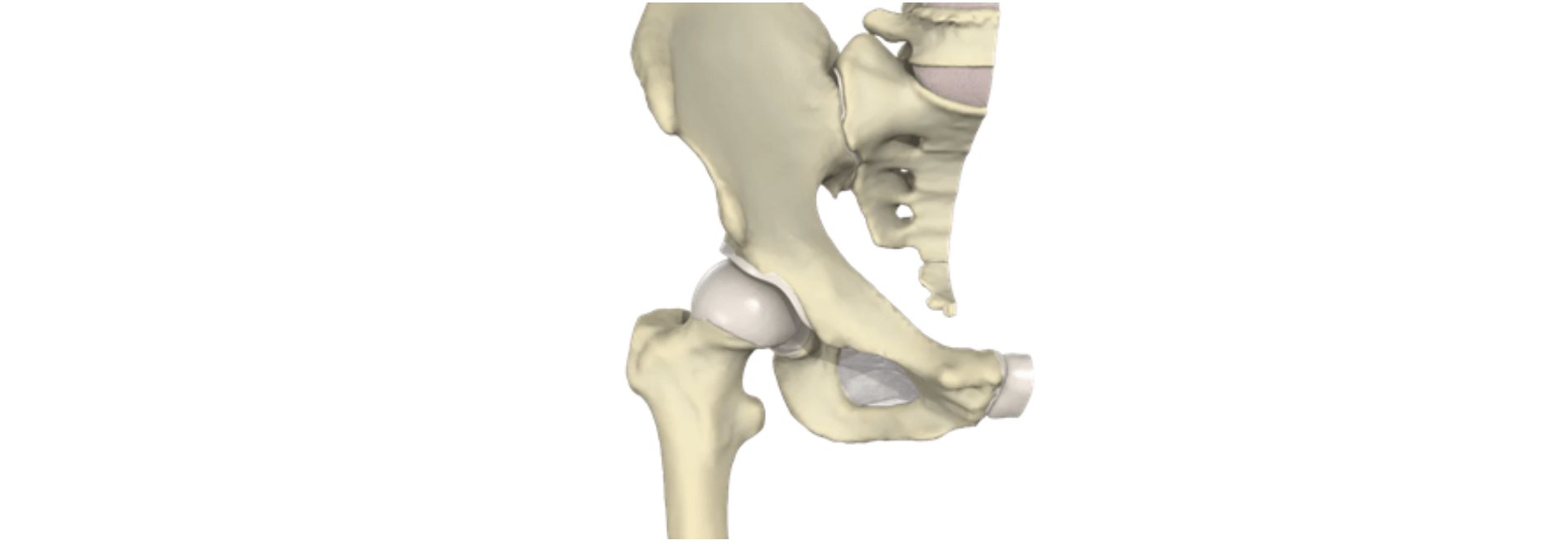
The hip joint is a ball & socket joint. The socket is part of the pelvis and the ball is part of the femur (thigh bone).
The socket is quite deep, which gives the hip great strength and stability.
In some people, the structure of the ball and socket can be variable:
- The socket can be extra deep, or twisted slightly backwards
- The ball can have some extra bone on the neck, which makes it hard for the ball to glide smoothly into the socket with movement.
Watch these videos to understand how these structural changes can affect the motion of the hip joint
These structural changes are one reason that you might suffer hip stiffness, and might potentially lead to a disorder know as FAI – Femor-acetabular impingement.
This type of hip stiffness might manifest during athletic movements such as hard cutting in a football game, deep squatting at the gym or cycling in an aerodynamic position.
Effective management of structural hip stiffness can involve modifying provocative activities, rehab strengthening, while at times it might require a surgical opinion. This all depends on the level of activity that the hip is required to achieve.
The second type of hip stiffness is that of our 8 hour / day desk worker.

Prolonged sitting causes a shortening across the front of the hip – What we know as “tight hip flexors”. At the same time the gluteal muscles are lengthened and can take a bit of a holiday!
Alternating your position to stand regularly or sitting on a higher chair can also help this group.
Sometimes we also suggest using a downslope chair, which will open the front of the hips more.
The third group of hip stiffness is a little paradoxical!
This is the group who actually have extra hip mobility – What we term hypermobility.
This is typical of adolescent females who are dancers, gymnasts etc.
The extra mobility can be a direct cause of a very shallow socket and lead to hip instability.
It seems counter-intuitive that this group would feel stiff, however this increase in hip mobility causes a strain on the bigger muscles around the hip, causing them to become overactive and produce a feeling of stiffness.
STRETCHING WILL NOT WORK! And may only irritate the hip joint.
Rather, some soft tissue release and deep hip stability exercises are the way to manage this group.
The final type of hip stiffness is the baby boomer generation who have developed Osteoarthritis (OA).
OA is a condition that we all experience to varying degrees as a natural part of the ageing process. The progression of OA can produce reductions in hip joint mobility – The hip feels stiff!
Effective management involves hip mobility & stability exercises with a general strength program, while understanding the limitations of the arthritic hip.
However, as we are finding with most joints that suffer arthritis on scan, the degree of arthritis does not correlate with pain. Some people have advanced cartilage changes and are still functioning at a really high level with minimal pain.
Alleviating your hip stiffness requires a very individualized approach. As demonstrated from the hip instability group, giving blanket hip flexor stretches to everyone is not the answer, and can lead to problems.
If you can empathise with one of the above categories, get an expert assessment with one of our leading Sports Physios.
It is then you will be free to shake your hips like our Colombian Queen of latin music!